Updated Guidelines to Reduce Maternal Mortality from Postpartum Hemorrhage
Let’s be honest, when we talk about childbirth, the focus is often on the miracle of new life. But what about the very real risks that mothers face? Postpartum hemorrhage (PPH) – excessive bleeding after childbirth – is a leading cause of maternal mortality worldwide, and sadly, India is no exception. Now, here’s the thing: updated guidelines are aiming to change that. But why now? And what makes these guidelines different? That’s what we’re diving into today.
Why These Updated Guidelines Matter | A Matter of Life and Death
I initially thought, “Okay, another set of guidelines, what’s the big deal?” But then I started digging. These aren’t just tweaks; they represent a fundamental shift in how we approach PPH. The ‘why’ behind these guidelines is deeply rooted in addressing systemic issues within our healthcare system. Think about it: access to quality prenatal care, availability of essential medicines, and well-trained healthcare providers aren’t uniform across India. This disparity directly impacts maternal mortality rates.
The updated guidelines aim to standardize protocols, ensuring that every woman, regardless of her location or socioeconomic status, receives the best possible care. We’re talking about earlier detection, more effective treatments, and better resource allocation. It’s about equity. It’s about saving lives that shouldn’t be lost. And that, my friend, is why these guidelines matter so much.
One key area is the emphasis on active management of the third stage of labor. This involves using uterotonic drugs (like oxytocin) immediately after delivery to help the uterus contract and prevent excessive bleeding. It sounds simple, but consistent implementation across all healthcare facilities is the challenge.
The ‘How’ | Implementing the Changes on the Ground
So, how will these guidelines actually translate into tangible improvements? It’s not enough to just publish a document; we need to see real changes on the ground. A common mistake I see is that guidelines are often disseminated without adequate training and support for healthcare workers. Imagine being a nurse in a rural health center, already stretched thin, and now you’re expected to implement a whole new set of protocols without proper training. It’s a recipe for failure.
The updated guidelines must be accompanied by comprehensive training programs, focusing on early detection of PPH, timely administration of medications, and effective management of complications. This includes simulation exercises, hands-on workshops, and ongoing mentorship programs. The one thing you absolutely must remember when administering oxytocin is the dosage – too much can be harmful. Regular refresher courses are also vital to ensure that healthcare providers stay up-to-date with the latest evidence-based practices.
Furthermore, these guidelines need to be integrated into existing healthcare systems, with clear lines of responsibility and accountability. We need to move beyond a siloed approach and foster collaboration between different departments and levels of care. This means streamlining referral pathways, ensuring timely access to blood transfusions, and establishing robust monitoring and evaluation mechanisms.
Addressing the Emotional Toll | The Forgotten Victims
Let me rephrase that for clarity – the impact of postpartum hemorrhage extends far beyond the physical realm. It leaves emotional scars on mothers, families, and even healthcare providers. That moment of panic when bleeding doesn’t stop; we can only imagine how traumatic this is.
The updated guidelines should also address the psychological support needed for women who experience PPH. This includes counseling services, peer support groups, and mental health screening. It’s not just about stopping the bleeding; it’s about helping women heal emotionally and regain their confidence.
And let’s not forget the healthcare providers who witness these events. They often carry the weight of responsibility and can experience vicarious trauma. Providing them with support and resources is crucial for their well-being and their ability to continue providing quality care.
Looking Ahead | Challenges and Opportunities
While these updated guidelines represent a significant step forward, several challenges remain. One major hurdle is the lack of reliable data on PPH incidence and outcomes in India. Without accurate data, it’s difficult to track progress, identify hotspots, and allocate resources effectively. Investing in robust surveillance systems is essential.
Another challenge is ensuring equitable access to essential medicines and technologies. Oxytocin, misoprostol, and tranexamic acid are life-saving drugs for managing PPH, but they are not always readily available in all healthcare facilities, particularly in rural areas. Strengthening supply chains and ensuring affordability are critical. According to the latest data from the Ministry of Health and Family Welfare, access to these medications varies significantly across states.
But amid these challenges, there are also opportunities. The increasing use of mobile technology and telemedicine can help improve access to antenatal care and facilitate early detection of risk factors for PPH. Community health workers can play a vital role in educating women about PPH prevention and promoting timely referral to healthcare facilities.
The Bottom Line | A Collective Responsibility
Ultimately, reducing maternal mortality from postpartum hemorrhage is a collective responsibility. It requires the commitment of governments, healthcare providers, communities, and individuals. The updated guidelines provide a framework for action, but their success depends on our willingness to implement them effectively, monitor their impact, and adapt them as needed.
Let’s be the generation that finally turns the tide on maternal mortality . Let’s ensure that every woman in India has the chance to experience the joy of motherhood without the fear of losing her life. And for those looking for more information on maternal health services , you can often find resources through your local healthcare providers. PPH prevention strategies should be a key focus during prenatal visits.
Here’s to a healthier, safer future for mothers in India. It’s not just about guidelines; it’s about making a real difference in people’s lives. And what fascinates me is how small changes can create a ripple effect that transforms healthcare.
FAQ Section
What exactly is postpartum hemorrhage (PPH)?
Postpartum hemorrhage (PPH) is defined as excessive bleeding after childbirth, typically more than 500 ml after a vaginal birth or more than 1000 ml after a C-section.
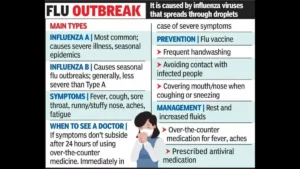
What are the common causes of PPH?
Common causes include uterine atony (failure of the uterus to contract), retained placental tissue, tears in the birth canal, and blood clotting disorders.
How can PPH be prevented?
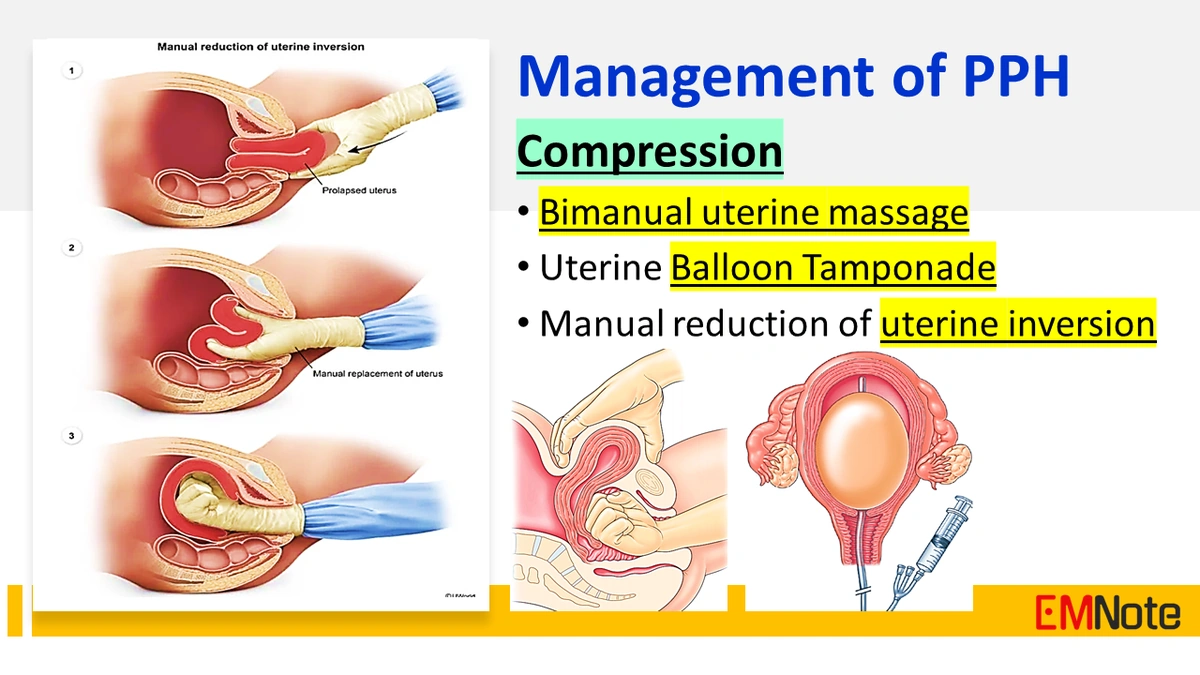
PPH can be prevented through active management of the third stage of labor, including the use of uterotonic drugs like oxytocin, controlled cord traction, and uterine massage.
What are the first steps if PPH occurs?
The first steps include calling for help, assessing the woman’s condition, massaging the uterus, administering uterotonic drugs, and initiating fluid resuscitation.
Where can I find more information about these guidelines?
Consult with your healthcare provider or refer to the official website of the Ministry of Health and Family Welfare for detailed information on the updated guidelines.
Are there any long-term effects of PPH?
Yes, PPH can lead to long-term complications such as anemia, fatigue, psychological trauma, and in severe cases, organ damage or death. Prompt and effective management is crucial.