First Nation Achieves Elimination of Mother-to-Child HIV, Hepatitis B, and Syphilis Transmission
Okay, folks, this isn’t just another news story; it’s a monumental achievement that deserves a deeper look, especially for us in India. A First Nation – an indigenous community – has successfully eliminated mother-to-child transmission of HIV, Hepatitis B, and Syphilis. Sounds amazing, right? But why is this so important, and what lessons can we draw from their success? Let’s dive in.
Why This Matters – A Global Perspective on Mother-to-Child Transmission Elimination
Here’s the thing: mother-to-child transmission is a huge problem globally. Think about it – a child’s life potentially compromised before it even truly begins. In many parts of the world, including some regions in India, access to prenatal care, testing, and treatment is limited. This First Nation’s achievement isn’t just a local victory; it’s a beacon of hope, showing what’s possible with focused effort and community involvement. The success offers important lessons on healthcare accessibility and cultural sensitivity, crucial aspects often overlooked in public health programs. The lessons learned are scalable and transferable, offering a blueprint for other communities, even those facing different challenges. We’ve got to ask ourselves, how can these strategies be adapted and implemented in our own diverse and challenging healthcare landscape?
And, it’s not just about the immediate health benefits. Think of the long-term impact on society. Healthier children grow into healthier adults, contributing more to their communities and the economy. It’s a virtuous cycle that starts with preventing transmission in the first place.
How Did They Do It? Unpacking the Strategies for MTCT Elimination
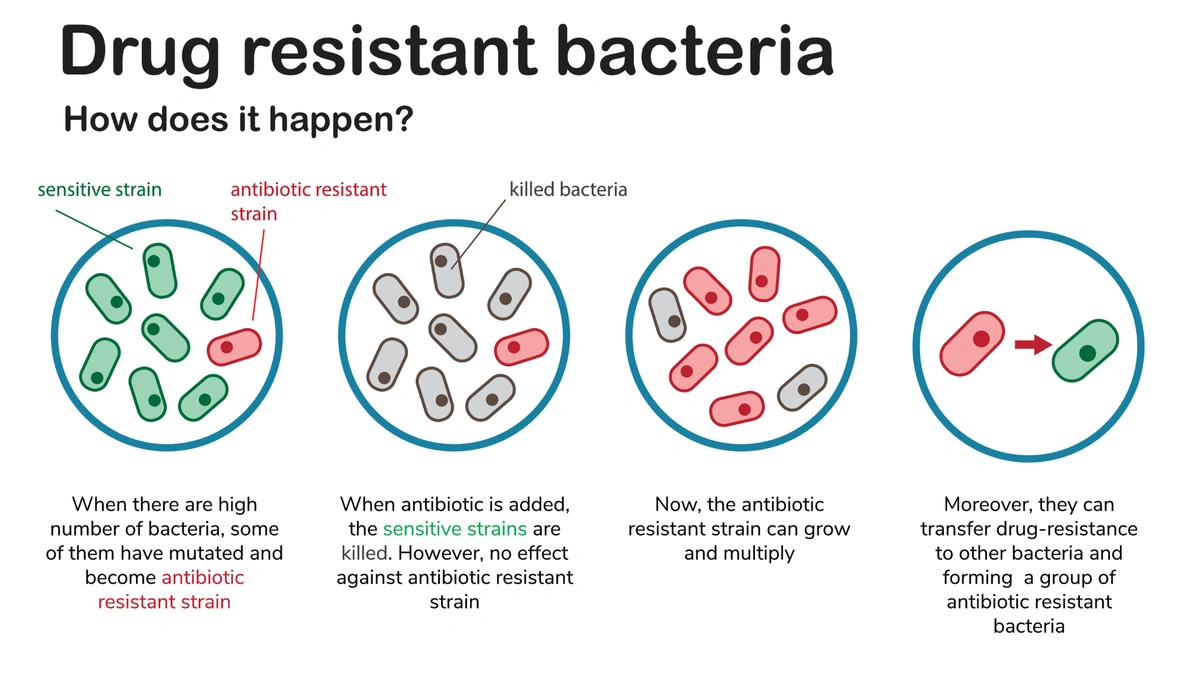
So, how did they pull it off? That’s the million-dollar question, isn’t it? While specifics vary depending on the community and their resources, several key elements are typically involved:
- Early and Consistent Prenatal Care: Regular check-ups allow for early detection and intervention.
- Universal Screening: Testing all pregnant women for HIV, Hepatitis B, and Syphilis.
- Effective Treatment: Providing antiretroviral therapy for HIV-positive mothers, vaccination against Hepatitis B, and antibiotics for Syphilis.
- Safe Delivery Practices: Implementing strategies to minimize the risk of transmission during childbirth.
- Infant Care and Follow-Up: Ensuring infants receive necessary vaccinations and monitoring for infection.
These measures are evidence based. According to the World Health Organization (WHO guidelines), implementing these strategies can significantly reduce the risk of mother-to-child transmission . But the real secret sauce? Community involvement. Programs must be culturally sensitive and tailored to the specific needs of the community. This involves working closely with local leaders, healthcare providers, and community members to build trust and ensure that services are accessible and acceptable.
The Emotional Angle: Hope and Empowerment in the Fight Against Congenital Infections
Let’s be honest – statistics and strategies can feel a bit detached. Behind every successful elimination, there are countless individual stories of hope, resilience, and empowerment. Imagine being a pregnant woman living in a remote community, facing the fear of potentially passing on a life-threatening infection to your child. Then, imagine having access to quality care, support, and the knowledge that you can protect your baby. That’s the power of MTCT elimination .
It’s a story of overcoming challenges, breaking down barriers, and creating a healthier future for generations to come. It’s a reminder that progress is possible, even in the face of adversity. And what fascinates me is that empowerment is essential. Women who are informed and supported are more likely to seek care and adhere to treatment, leading to better outcomes for themselves and their children.
Lessons for India: Scaling Up PMTCT Programs
So, what can India learn from this achievement? A lot, actually. While India has made significant progress in reducing mother-to-child transmission , challenges remain. Unequal access to healthcare, stigma surrounding HIV and other infections, and limited awareness are all factors that hinder progress. As discussed on dengue in india , addressing health disparities in India requires a multi-pronged approach, from improving infrastructure to launching targeted awareness campaigns.
We need to:
- Strengthen primary healthcare systems to ensure access to prenatal care for all women.
- Scale up testing and treatment programs, particularly in underserved areas.
- Address stigma and discrimination to encourage people to seek care.
- Promote community involvement and empower women to take control of their health.
I initially thought this was straightforward, but then I realized… it’s about more than just medical interventions. It’s about creating a society where every child has the opportunity to thrive, regardless of their mother’s health status. As highlighted in the article about innovative cancer treatments , pushing the boundaries of science and technology requires political will and resources.
Funding and Resources for Pediatric HIV/AIDS
Let’s talk brass tacks – none of this happens without resources. Sustained funding is essential to maintain progress and prevent resurgence. This includes investments in healthcare infrastructure, training of healthcare providers, and procurement of essential medicines and supplies. Furthermore, the use of data for decision-making and program improvement is vital. Regular monitoring and evaluation can help identify gaps in service delivery and ensure that resources are being used effectively. It’s a cycle of continuous improvement, driven by a commitment to evidence-based practice.
FAQ: Addressing Common Concerns About Vertical Transmission
What if I am pregnant and test positive for one of these infections?
Don’t panic! With proper medical care, the risk of transmitting the infection to your baby can be significantly reduced. Follow your doctor’s instructions carefully.
How early in pregnancy can I get tested?
Ideally, you should get tested as early as possible in your pregnancy to allow for timely intervention.
Are these tests expensive?
Many public health programs offer free or subsidized testing for pregnant women. Check with your local healthcare provider.
What happens if my baby tests positive after birth?
Early diagnosis and treatment can help your baby live a healthy life. Follow your doctor’s recommendations closely.
Where can I find more information and support?
Contact your local healthcare provider, public health department, or organizations specializing in maternal and child health. You can also find more information at the Centers for Disease Control (CDC website).
Ultimately, the elimination of mother-to-child transmission is a testament to the power of science, compassion, and community. It’s a journey, not a destination, requiring continuous effort and commitment. But the rewards – healthy children, thriving families, and a brighter future – are immeasurable. And that’s something worth fighting for, don’t you think?