Cough Syrup Contamination | Regulatory Loopholes Highlight the Importance of Global Standards
The headlines scream: contaminated cough syrups, children harmed, even deaths reported. It’s a parent’s worst nightmare, honestly. But beyond the initial shock, a more profound question lingers: why does this keep happening? We’re not talking about isolated incidents anymore. This is a recurring tragedy, and it points to a systemic failure – a failure to enforce robust global standards in the pharmaceutical industry. Let’s be honest, the current system feels like a game of whack-a-mole, addressing problems only after they explode into the public consciousness. But why? And more importantly, what can we do to change it? This isn’t just about pointing fingers; it’s about understanding the gaps and advocating for a safer future.
The Labyrinth of Lax Regulations and Its Deadly Consequences

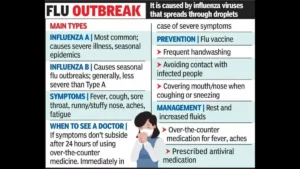
Here’s the thing: the global pharmaceutical supply chain is incredibly complex. Ingredients and finished products crisscross borders multiple times, often passing through countries with varying levels of regulatory oversight. This creates opportunities for unscrupulous manufacturers to cut corners, using substandard or even toxic ingredients. The recent incidents of cough syrup contamination highlight the devastating consequences of these regulatory loopholes . We’re talking about children, often the most vulnerable, being exposed to dangerous levels of diethylene glycol (DEG) and ethylene glycol (EG) – industrial solvents that are absolutely not meant for human consumption. But, it’s not always about malice. Sometimes, it’s sheer negligence, a lack of rigorous testing, and a failure to adhere to good manufacturing practices (GMP). The question is, who’s watching the watchers? The pharmaceutical industry has a responsibility, but so do governments and international organizations.
Global Harmonization | A Utopian Dream or a Necessary Reality?
The answer, in my opinion, lies in greater global harmonization of pharmaceutical regulations. Think about it: if every country adhered to the same rigorous standards for quality control, testing, and manufacturing, it would be much harder for substandard products to slip through the cracks. But achieving this level of harmonization is a monumental task. Different countries have different priorities, different resources, and different political landscapes. Some may resist efforts to align their regulations with international standards, fearing it could hurt their domestic industries or create barriers to trade. And, let’s not forget the power of lobbying from certain players who benefit from the status quo. Yet, the cost of inaction is far too high. We’re talking about lives – children’s lives. So, what are the specific obstacles, and how can we overcome them? One key aspect is strengthening regulatory agencies in countries with weaker oversight. This means providing them with the resources, training, and technology they need to effectively monitor pharmaceutical manufacturing and supply chains.
The Indian Context | Balancing Affordability and Safety
India, as one of the world’s largest manufacturers of generic drugs, has a crucial role to play in ensuring the safety of pharmaceuticals. While India has made significant strides in strengthening its regulatory framework, challenges remain. The sheer scale of the Indian pharmaceutical industry, with its thousands of manufacturers and complex supply chains, makes it difficult to monitor every single product. Moreover, the pressure to keep drug prices affordable can sometimes lead to compromises on quality. This is a delicate balancing act – providing access to affordable medicines while ensuring that those medicines are safe and effective. What fascinates me is how we can achieve this balance? We need to ensure that Indian pharmaceutical manufacturers adhere to the highest international standards, not just for export markets, but also for domestic consumption. Increased pharmaceutical quality control and investment in advanced testing facilities are essential. Also, fostering a culture of transparency and accountability within the industry is critical. Navigating regulatory landscapes can be tricky but is essential for manufacturers and distributors alike.
The Role of International Organizations and Collaborative Efforts
No single country can solve this problem alone. International organizations like the World Health Organization (WHO) have a vital role to play in coordinating global efforts to combat cough syrup contamination incidents . The WHO can provide technical assistance to countries with weaker regulatory systems, develop and promote international standards for pharmaceutical manufacturing, and facilitate the sharing of information and best practices. But the WHO’s efforts can only be effective if they are supported by strong political will from member states. This means committing resources, enacting legislation, and enforcing regulations. It also means fostering a culture of collaboration and information-sharing among countries, regulatory agencies, and pharmaceutical manufacturers. Increased global health security is not just a buzzword; it’s a necessity in an interconnected world.
But, even with the best regulations and oversight, mistakes can still happen. That’s why it’s also crucial to have effective mechanisms for detecting and responding to drug safety alerts . This includes establishing robust surveillance systems to monitor adverse drug events, developing rapid alert systems to warn the public about potentially contaminated products, and having effective recall procedures to remove dangerous drugs from the market. Let me rephrase that for clarity: it’s not enough to just prevent contamination; we also need to be prepared to deal with it when it occurs. And risk assessment is also important because this means identifying potential vulnerabilities in the supply chain and taking proactive steps to mitigate them.
Conclusion | A Call for Vigilance and Action
The issue of cough syrup contamination is a stark reminder of the importance of global standards and regulatory oversight in the pharmaceutical industry. It’s a call for vigilance, for action, and for a collective commitment to protecting the health and safety of our children. We can’t afford to be complacent. We must demand greater transparency, stronger regulations, and more effective enforcement. The next time you reach for a bottle of cough syrup, remember that it’s not just a medicine; it’s a product of a complex global supply chain, and its safety depends on the integrity of that chain. Let’s work together to ensure that every child, everywhere, has access to safe and effective medicines. The goal is to develop robust supply chains that are transparent, secure, and resilient.
FAQ
What exactly is diethylene glycol (DEG)?
DEG is an industrial solvent that is toxic to humans. It’s sometimes mistakenly used in place of safe ingredients like propylene glycol or glycerin in pharmaceutical products.
How can I be sure the medicines I buy are safe?
Always purchase medicines from reputable pharmacies and check for proper labeling and seals. If you have any concerns, consult with your doctor or pharmacist.
What are the signs of DEG poisoning?
Symptoms can include nausea, vomiting, abdominal pain, kidney failure, and neurological problems. Seek immediate medical attention if you suspect DEG poisoning.
What is being done to prevent future incidents of contamination?
Efforts are underway to strengthen regulatory oversight, improve quality control, and increase collaboration among countries and international organizations.
What role does the World Health Organization (WHO) play in all of this?
The WHO provides technical assistance, develops standards, and facilitates information sharing to help countries ensure the safety of pharmaceutical products.
Where can I find up-to-date information on drug safety alerts?
Check the websites of your national regulatory agency (e.g., the CDSCO in India) and the WHO for the latest alerts and advisories. And check out relevant articles and resources .