Alarming Antibiotic Resistance | WHO 2025 Report Highlights India’s Struggle. Experts Urge Reforms. #AntibioticResistance #WHO2025 #GlobalHealth #AMR
Here’s the thing: we’ve all heard about antibiotic resistance . It sounds scary, right? Like something out of a sci-fi movie where superbugs take over the world. But what does it really mean for you, sitting in India, just trying to stay healthy? The recent WHO 2025 report shines a stark light on India’s struggle with this growing problem. And honestly, it’s not just a headline; it’s a wake-up call. So, let’s dive into why this matters, shall we?
Understanding the Crisis | More Than Just Headlines
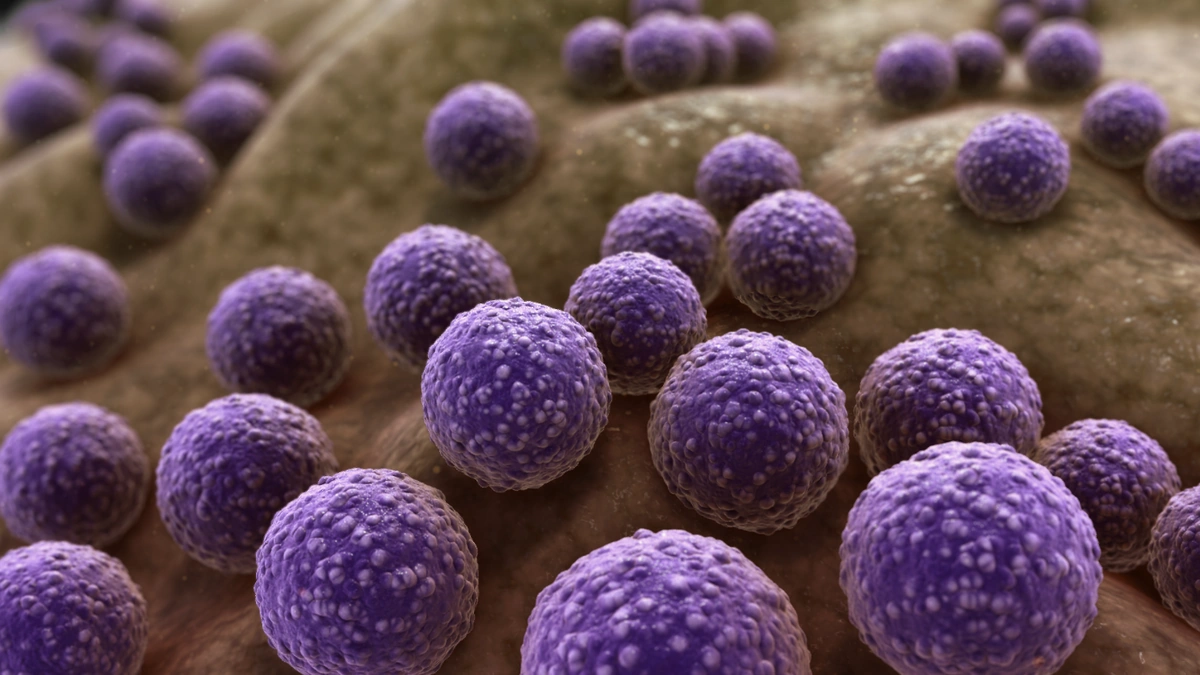
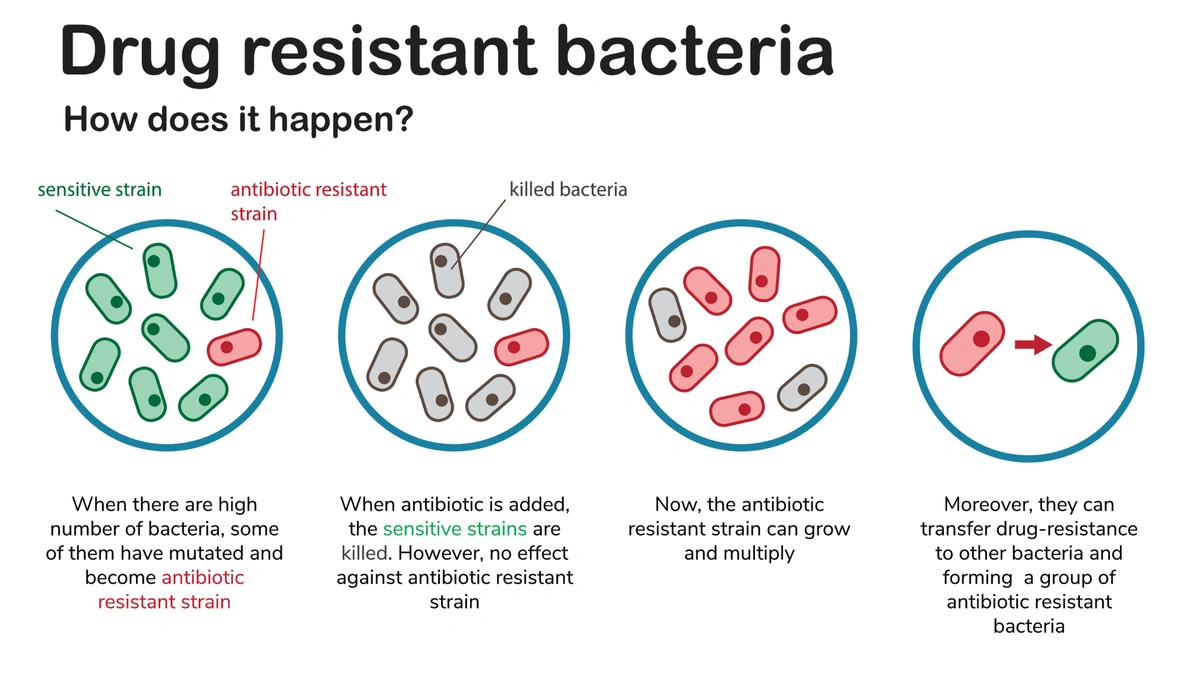
Okay, so the WHO report. It paints a picture. A concerning one. It doesn’t just say, “India has a problem with AMR (Antimicrobial Resistance).” It shows how we’re potentially facing a future where common infections become life-threatening again. Imagine a simple cut turning into a nightmare because the antibiotics you’d normally take just…don’t work. That’s the reality we’re staring down.
But, why is India particularly vulnerable? Well, several factors are at play. Over-the-counter availability of antibiotics is a big one. You can often walk into a pharmacy and get antibiotics without a prescription. Easy access, right? Not always. This fuels overuse and misuse, creating a breeding ground for resistant bacteria. Another piece of the puzzle is sanitation. Suboptimal sanitation and hygiene practices, especially in densely populated areas, contribute to the spread of bacteria. As per the guidelines mentioned in the information bulletin about AMR. This situation is exacerbated by the misuse of antibiotics in agriculture and animal husbandry, leading to the development of antibiotic resistant bacteria that can then spread to humans.
I initially thought this was straightforward – a matter of overuse. But then I realized the complexity. It’s a tangled web of social, economic, and infrastructural issues. As Deepika Padukone emphasizes the importance of proactive healthcare, we too must emphasize the need to tackle the antibiotic resistance threat with urgency.
What You Can Do | A Practical Guide
So, what can you actually do? Feels overwhelming, I know. But here’s the thing: individual actions add up. This is not just a problem for the government or doctors to solve. We all have a role to play.
- Don’t self-medicate. This is huge. Resist the urge to pop antibiotics for every sniffle. Trust your doctor to determine if they’re truly necessary.
- Complete the full course. If a doctor does prescribe antibiotics, finish the entire course, even if you feel better. Stopping early allows stronger bacteria to survive and develop resistance.
- Practice good hygiene. Wash your hands frequently with soap and water, especially after using the restroom and before eating. It sounds basic, but it’s incredibly effective.
- Be a responsible consumer. Support farmers and food producers who use antibiotics responsibly in their animals.
A common mistake I see people make is thinking that antibiotics are a cure-all. They’re not. They only work against bacterial infections, not viruses like the common cold or flu. Remember that! The overuse of antibiotics to treat viral infections is a major contributor to the growth of antibiotic-resistant strains .
Let me rephrase that for clarity: antibiotics are not your friend when you have a viral infection.
The Looming Threat | Potential Consequences
What happens if we don’t get a handle on this? The consequences are far-reaching and, frankly, terrifying. Increased mortality rates from common infections are just the beginning. More expensive treatments, longer hospital stays, and a potential collapse of modern medicine are all on the table.
Think about surgeries, for example. Many rely on antibiotics to prevent post-operative infections. If those antibiotics stop working, the risks associated with surgery skyrocket. Or consider chemotherapy, which weakens the immune system, making patients highly vulnerable to infections. Antimicrobial resistance could severely limit the effectiveness of these life-saving treatments. Beyond the health implications, there are also economic consequences. Increased healthcare costs, reduced productivity, and a potential drag on economic growth are all possibilities. According to the latest circular on the official NTA website , this is something that requires immediate attention from all stakeholders.
Expert Insights | Calls for Urgent Action
It’s not all doom and gloom, though. Experts are calling for urgent reforms, and there’s a growing awareness of the problem. The WHO is pushing for global action plans to combat antimicrobial resistance , and many countries are implementing strategies to promote responsible antibiotic use. The Indian government has also launched initiatives to raise awareness and regulate the sale of antibiotics. For instance, the National Action Plan on Antimicrobial Resistance (NAP-AMR) outlines strategies for infection prevention and control, antimicrobial stewardship, and surveillance of AMR.
What fascinates me is the potential for innovation. Scientists are working on new types of antibiotics and alternative therapies to combat resistant bacteria. Phage therapy, which uses viruses to target bacteria, is one promising avenue. Developing rapid diagnostic tests to quickly identify infections and determine antibiotic susceptibility is another crucial step. These kinds of tests can help prevent unnecessary antibiotic use and ensure that patients receive the most effective treatment.
India’s Path Forward | Reforms and Responsibility
So, where do we go from here? India needs a multi-pronged approach that involves government regulations, public awareness campaigns, and individual responsibility. Strengthening surveillance systems to track resistance patterns and identify emerging threats is essential. Implementing stricter regulations on the sale and use of antibiotics is also crucial. But perhaps most importantly, we need to change the way we think about antibiotics. They are not a commodity to be used casually, but a precious resource that must be protected.
But, it’s about more than just rules and regulations. It’s about education, about changing attitudes, and about fostering a sense of collective responsibility. It’s about empowering individuals to make informed decisions about their health and the health of their communities. The link here shows how crucial it is to always remain aware of any medical updates.
The fight against antibiotic resistance is a marathon, not a sprint. It requires sustained effort, collaboration, and a willingness to adapt and innovate. But with commitment and determination, we can protect this valuable medicine and secure a healthier future for all.
Frequently Asked Questions (FAQ)
What exactly is antibiotic resistance?
It’s when bacteria evolve and become resistant to antibiotics, making infections harder or impossible to treat.
Why is antibiotic resistance a problem?
It can lead to longer illnesses, more hospitalizations, and increased risk of death.
How can I prevent antibiotic resistance?
Don’t self-medicate, complete the full course of antibiotics if prescribed, practice good hygiene, and be a responsible consumer.
What is India doing to combat antibiotic resistance?
The Indian government has launched initiatives to raise awareness and regulate the sale of antibiotics.
Are there alternatives to antibiotics?
Scientists are exploring phage therapy and other alternative therapies to combat resistant bacteria.
Where can I learn more about antibiotic resistance?
You can visit the WHO website or consult your doctor for more information.
Here’s the final insight: The fight against antibiotic resistance isn’t just a medical issue; it’s a societal one. It demands a fundamental shift in how we perceive and use these life-saving drugs. It’s a test of our collective responsibility, and the stakes couldn’t be higher.